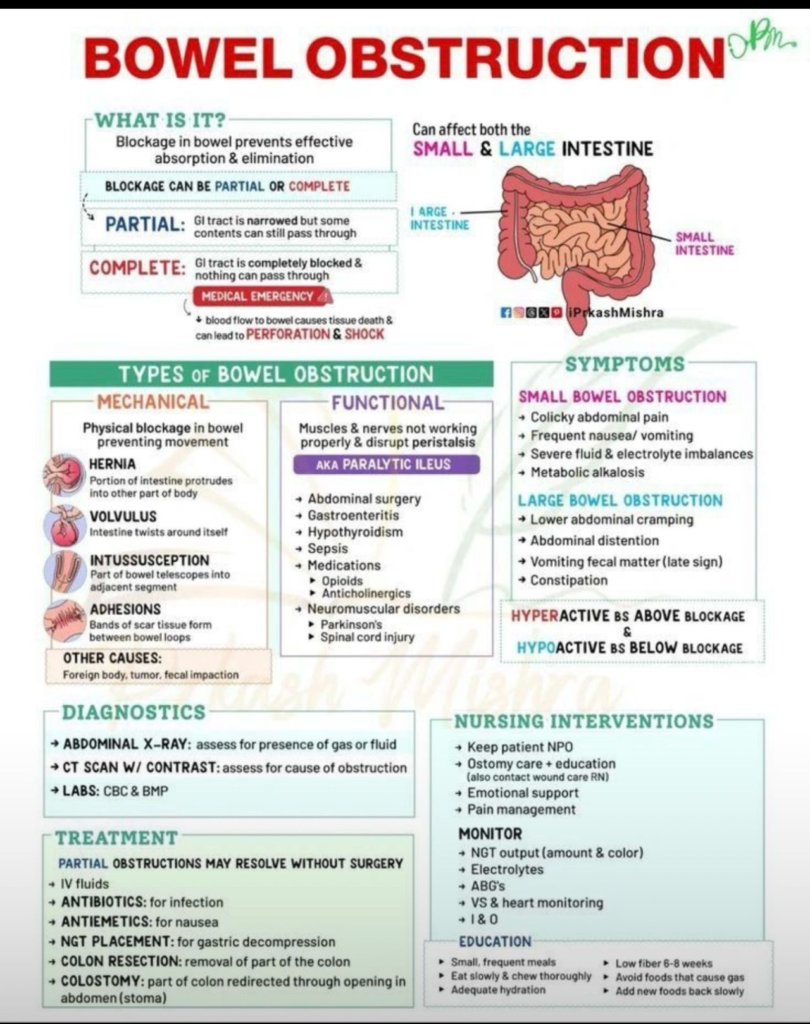
Bowel obstruction is a serious medical condition in which a blockage in the intestine prevents effective absorption and elimination of food and waste. This blockage can occur in both the small and large intestines, and it may be either partial or complete.
Prompt recognition and management of bowel obstruction are essential, as complete obstruction is a medical emergency that can lead to severe complications like tissue death, perforation, and shock.
Contents
What Is Bowel Obstruction?
Bowel obstruction refers to the narrowing or complete blockage of the gastrointestinal (GI) tract. There are two main types:
- Partial Obstruction: The GI tract is narrowed, so some content can still pass through.
- Complete Obstruction: The GI tract is entirely blocked, and nothing can pass. This condition demands urgent medical attention due to the risk of severe complications.
Obstruction impedes the normal movement of food, fluids, and gas, affecting the body’s ability to absorb nutrients and eliminate waste efficiently.
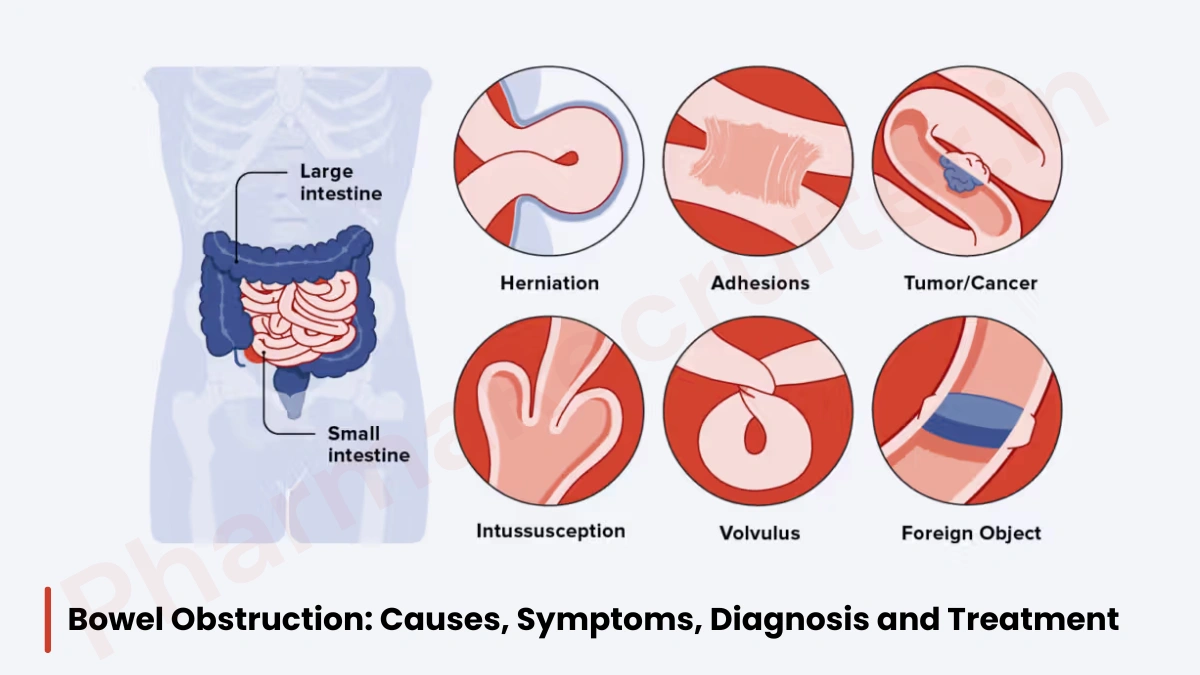
Types of Bowel Obstruction
Bowel obstruction can be categorized into two broad types: mechanical and functional.
Mechanical Obstruction
This type involves a physical blockage that prevents bowel movement. Common causes include:
- Hernia: Protrusion of the intestine into another part of the body.
- Volvulus: Intestine twists around itself.
- Intussusception: Part of the bowel telescopes into an adjacent segment.
- Adhesions: Bands of scar tissue form between bowel loops.
- Other causes: Foreign bodies, tumors, or fecal impaction.
Functional Obstruction (Paralytic Ileus)
Here, the muscles and nerves are not working properly, disrupting normal peristalsis. Common reasons include:
- Previous abdominal surgery
- Gastroenteritis
- Hypothyroidism
- Sepsis
- Certain medications (e.g., opioids, anticholinergics)
- Neuromuscular disorders like Parkinson’s disease or spinal cord injuries
Common Symptoms of Bowel Obstruction
Symptoms may differ depending on whether the obstruction is in the small or large bowel.
Small Bowel Obstruction:
- Severe, colicky abdominal pain
- Frequent nausea or vomiting
- Severe fluid and electrolyte imbalances
- Metabolic alkalosis
Large Bowel Obstruction:
- Lower abdominal cramping
- Abdominal distention
- Vomiting (especially of fecal matter in late stages)
- Constipation
A notable sign is hyperactive bowel sounds above the site of the blockage, while bowel sounds are hypoactive below the obstruction.
Diagnostic Strategies
Diagnosing bowel obstruction involves:
- Abdominal X-ray: Identifies the presence of gas or fluid.
- CT Scan with Contrast: Pinpoints the exact location and cause of the blockage.
- Lab Tests: Complete blood count (CBC) and basic metabolic profile (BMP) help assess patient stability.
Treatment Options
Partial obstructions may resolve without surgery, requiring:
- IV fluids
- Antibiotics if infection is present
- Antiemetics for nausea
- Nasogastric tube (NGT) placement for gastric decompression
For complete or severe obstructions, surgical intervention may be necessary, including:
- Colon resection (removal of the affected part)
- Colostomy (redirection of the colon through the abdomen)
Nursing Interventions and Patient Education
Care for patients with bowel obstruction includes keeping the patient NPO (nothing by mouth), ostomy care, pain management, monitoring output from tubes and vital signs, and ensuring adequate hydration.
Patients are encouraged to consume small, frequent meals and avoid high-fiber foods for the first 6–8 weeks after treatment. Eating slowly and thoroughly, as well as staying hydrated, support digestive health during recovery.
Conclusion
Understanding the causes, symptoms, and treatments of bowel obstruction can help in early diagnosis and management. Timely intervention greatly reduces the risk of complications and improves patient outcomes.